“Tissue Engineering and Regenerative Medicine. Tissue engineering has evolved from the field of biomaterial development. It refers to the practice of combining scaffolds, cells, and biologically active molecules to create functional tissues. The goal of tissue engineering is to gather ideas or theories that restore, maintain, or improve damaged tissues or entire organs. The FDA has approved examples of engineered tissues such as artificial skin and artificial cartilage. It is important to highlight that they currently have limited use in human patients.
Regenerative medicine is a broad field that includes tissue engineering but also incorporates research on self-healing. It occurs when the body uses its systems, sometimes with the help of foreign biological material. To recreate cells and rebuild tissues and organs. The terms “tissue engineering” and “regenerative medicine” have become interchangeable. As the field aims to focus on cures rather than treatments for complex and often chronic diseases.
This field continues to evolve. In addition to medical applications, non-therapeutic applications include using tissues as biosensors to detect biological or chemical threats and tissue chips that we use to test the toxicity of an experimental drug.
How do tissue engineering and regenerative medicine work?
Cells are the fundamental components of tissue, and tissues are the basic unit of function in the body. Generally, groups of cells form and secrete their support structures, called the extracellular matrix. This matrix, or scaffold, does more than just serve as support for cells; it also acts as a repeater station for various signaling molecules. Thus, cells receive messages from many sources made available from the local environment. Each signal can initiate a chain of responses that determine what happens to the cell. By understanding how individual cells respond to signals, how they interact with their surroundings, and how they organize into tissues and organisms, researchers have been able to manipulate these processes to heal damaged tissues or even create new ones.
The process often begins with the construction of a scaffold from a wide range of possible sources, from proteins to plastics. Once scaffolds are created, cells can be introduced with or without a “cocktail” of growth factors. If the environment is suitable, tissue develops. In some cases, cells, scaffolds, and growth factors are all mixed at the same time, allowing the tissue to “self-assemble.”
Another method to create new tissue uses an existing scaffold. Cells from a donated organ are removed, and the remaining collagen scaffold is used to grow new tissue. This process has been used for tissue engineering of the heart, liver, lung, and kidney. This approach offers great hope for using scaffolding with discarded human tissue during surgery and combining it with a patient’s cells to make customized organs that are not rejected by the immune system.
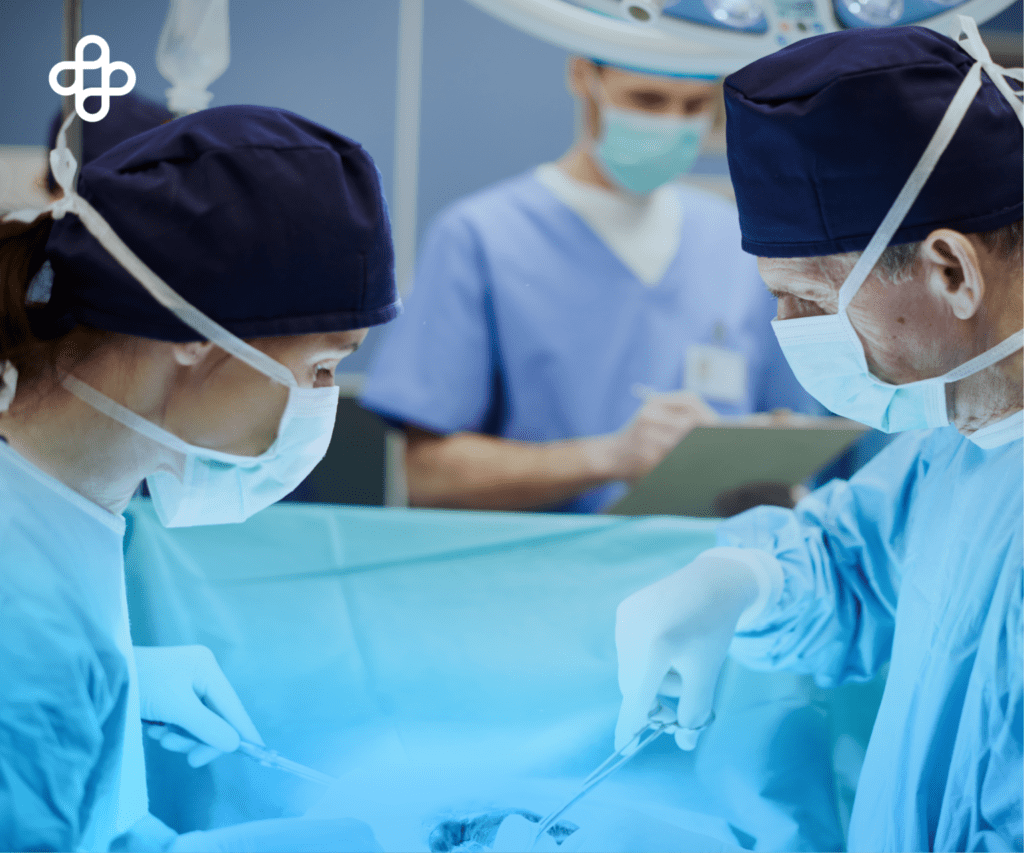
How do tissue engineering and regenerative medicine fit into current medical practices?
According to the NIH, tissue engineering currently plays a relatively small role in patient treatment. Supplementary bladders, small arteries, skin grafts, cartilage, and even a complete trachea have been implanted in patients. However, the procedures are still experimental and very costly. While more complex organ tissues such as the heart, lung, and liver have been successfully recreated in the laboratory. hey are still far from being fully reproducible and ready for implantation in a patient. However, these tissues can be highly useful in research, especially in drug development. By using functional human tissue to help select drugs, candidates could expedite development and provide key tools to facilitate personalized medicine, saving money and reducing the number of animals used for research.
What are NIBIB-funded researchers developing in the areas of tissue engineering and regenerative medicine?
NIBIB-supported research includes the development of new scaffold materials and new tools for manufacturing, imaging, monitoring, and preserving engineered tissues. Below are some examples of research in this area:
- Stem Cell Control through Their Environment
- Implantation of Human Livers in Mice
- Creation of Mature Bone Stem Cells
- Use of Meshes to Help Engineered Tissue Survive
- New Hope for Injured Knees: Repairing cartilage has been challenging, if not impossible, due to the lack of a blood supply to promote regeneration. There has been a 50% long-term success rate using microfracture surgery in young adults with sports injuries, and little to no success in patients with widespread cartilage degeneration, such as osteoarthritis.
- Regeneration of a New Kidney
If you want to learn more about regenerative medicine, I invite you to read our article “What Is Regenerative Medicine?”